 An article, written by Principal Clinical Psychologist Colby Pearce, which originally appeared on Colby’s blog site Attachment and Resilience.
An article, written by Principal Clinical Psychologist Colby Pearce, which originally appeared on Colby’s blog site Attachment and Resilience.
In our practice one of the more common presenting problems is severe tantrums, or meltdowns, in children. Common reactions among adults who care for these children include frustration, embarrassment, desperation and helplessness. Typically, these otherwise competent parents have tried a range of strategies without finding a strategy or strategies that consistently work. They invariably pose one simple question: what do we do when our child is having a severe tantrum or meltdown? What they really want to know is, what works?
The first answer I provide is that there is no known universally effective strategy for managing severe tantrums and meltdowns. If there was, someone would have written about it by now and made a lot of money! The second answer I offer is that effective management of children’s severe tantrums and meltdowns begins with developing an understanding of what is actually going on in the nervous system of a child prior to, and in the midst of, a severe tantrum or meltdown.
The most common belief that exists in the community about severe tantrums and meltdowns is that they are a behaviour management problem. In fact, they are anarousal management problem. Understanding this is the key to effective management of meltdowns and severe tantrums.
By arousal, I mean the level of activity in the child’s nervous system. Arousal goes up and down during the day. Arousal generally is lowest when the child is asleep and highest when the child is in a state of high emotion. Arousal is regulated by the brain, though it is influenced by what the child is doing and what is happening in the child’s environment. In ordinary circumstances, arousal is thought to go up and down within a regular range, which varies from child to child. Each child’s range of arousal is affected by genetic factors (e.g. temperament), early exposure to stress, ongoing maintaining factors (i.e.stressors), and the interaction of these. The temperament infants are born with is involved, as so-called “easy babies” seemingly maintain lower levels of arousal, whereas so-called “slow-to-warm-up” and “difficult” babies maintain higher levels of arousal.
Early stressors include pregnancy and birth complications, early illness, neglect and maltreatment. Early stressors are thought to impact on the structure of the developing brain, particularly those structures that are responsible for the control, or regulation, of arousal[i]. Frequent exposure to stress and prolonged distress, particularly during the first year of life, is thought to result in significant development of the parts of the brain that are associated with high arousal and emotional distress. The result of this is that the central nervous system (i.e. the brain) becomes hard-wired to be highly reactive to sensory stimulation (i.e. sights, sounds, touch, taste, smell) and perceived threats, and vulnerable to maintaining higher levels of arousal. Maintaining factors include stressors associated with higher arousal, including bullying and harassment, learning difficulties and traumatic family circumstances. Maintaining factors also include strength factors that support lower arousal, such as the presence of loving and supportive relationships.
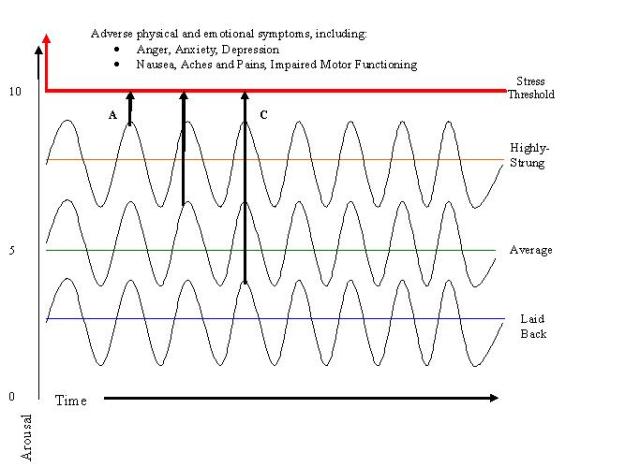
A conventional term for children whose arousal fluctuates in the higher range is that they are “highly strung”. Conversely, a conventional term for children whose arousal fluctuates in the lower range is that they are “laid back”. Highly strung children are on-the-go, intense, and make mountains out of molehills. Laid back children are comparatively relaxed, calm, unflappable and resilient. As is represented in the diagram below, it seems to take relatively more stimulation and adversity for laid back children to experience stress (C). In contrast, highly strung children are more prone to stress (A), and its associated negative consequences, than laid back children.
 (Source: Pearce, C. A Short Introduction to Promoting Resilience in Children. London: Jessica Kingsley, 2011)
(Source: Pearce, C. A Short Introduction to Promoting Resilience in Children. London: Jessica Kingsley, 2011)
Severe tantrums and meltdowns occur when a child’s arousal level approaches and exceeds the so-called stress threshold referred to in the above diagram. Brain imaging studies show that when an individual is under stress, or when an individual is exposed to sensory stimulation associated with past traumatic events, there is significant activation of sub-cortical (i.e. inner) regions of the brain and reduced blood flow to areas of the frontal cortex[i]’[ii] (i.e. outer, frontal regions of the brain). The areas of frontal cortex of the brain that experience reduced blood flow are thought to be those that are responsible for logical, rational thinking, planning and responding, and speech. The sub-cortical regions of the brain are responsible for instinctive responses and those that are essential to the survival of the organism, such as emotion, respiration, arousal and the fight-flight-freeze response.
Many behaviours exhibited by children during a severe tantrum or meltdown are associated with a reduced capacity for logical thinking and partial or full activation of the fight-flight-freeze response. These include controlling, aggressive, destructive, hyperactive and unreasonable behaviour. These behaviours are only partly volitional or totally non-volitional, depending on the child’s level of distress. The way in which parents (and other caregivers; e.g. teachers and childcare workers) respond to these behaviours either escalates (disciplinary response) or de-escalates (calming response) these behaviours.
So, when a child is having a severe tantrum or meltdown they require interventions that lower their arousal levels. It is only when we do so that the child will begin to behave in a more reasonable manner. I will present strategies for intervening to lower arousal and maintain lower arousal levels more generally in Taming Tantrums; Managing Meltdowns – Part Two.
(Note: much of the material presented in this article can is sourced from my various publications, including my two books: A Short Introduction to Attachment and Attachment Disorder and A Short Introduction to Promoting Resilience in Children.)
(Dislaimer: While it is anticipated that this article will prove to be informative for those who care for children, it is not a substitute for a full assessment and face-to-face support and guidance from an appropriately trained and experienced child development and mental health clinician. If your child is exhibiting severe and recurrent tantrums and meltdowns you should seek further advice about treatment options from your family medical practitioner).
[i] Perry, B.D., Pollard, R.A., Blakley, T.L., Baker, W.L., & Vigilante, D. (1995). Childhood trauma, the neurobiology of adaptation, and “use-dependent” development of the brain: How “states” Become “traits”, Infant Mental Health Journal, 16(4), 271-289
[ii] Damasio, A.R., Grabowski, T.J., Bechara, A., et al. (2000). Subcortical and cortical brain activity during the feeling of self-generated emotions. Nature Neuroscience, 3, 1049-1056
[iii] Van Der Kolk, B. (2006). Clinical implications of neuroscience research in PTSD.Annals of the New York Academy of Sciences, 1-17
